Almost 240,000 New Zealanders have been screened for cervical cancer at Awanui Labs – Dunedin, since HPV Primary Screening went live in September last year.
“Since September, Human Papillomavirus (HPV) testing has become the primary screening test for cervical cancer,” says Head of Molecular Pathology, Jenny Grant.
“HPV is responsible for the majority of cervical cancers, and testing for HPV can provide an earlier warning signal for people at higher risk of developing cervical cancer, than the previous cytology-based screening programme.”
Nearly 85 percent of adults will contract HPV at some point in their lives, and in most people an HPV infection clears itself within a couple of years. However, persistent HPV infections can lead to the development of cervical cancer.
“Screening for HPV can be performed on either a speculum-based cervical sample or a vaginal swab. These swabs are either self-collected by the patient, or taken by the patient’s clinician. This week, we hit a major milestone of processing over 100,000 of these swabs in 2024,” says Jenny.
“It was a huge unknown as to how many women would take up the option of a vaginal swab instead a speculum based cervical sample before the programme went live. However, the option of a vaginal swab has proved popular with approximately 75 percent of the samples received for HPV testing being from this swab.
“Part of the attraction for vaginal swabs is it is less invasive than having a speculum-based cervical sample taken.”
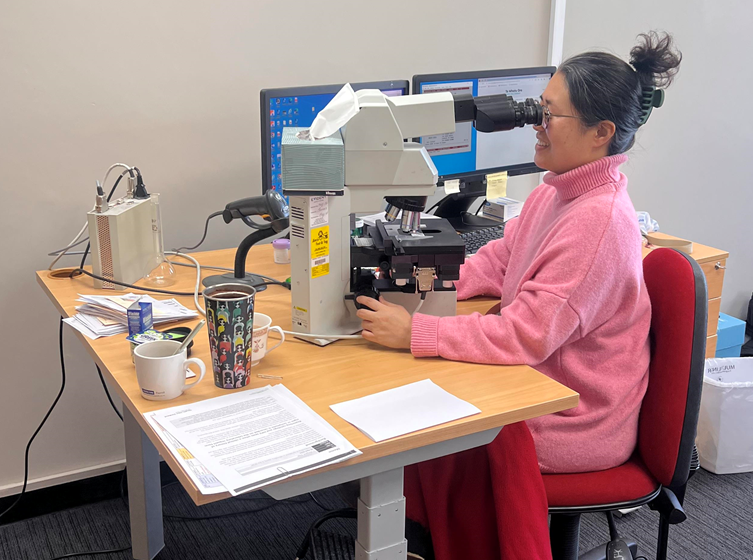
Following HPV testing, cytology is performed to look for cellular changes in those people in which HPV has been detected, or in those women who are experiencing signs and symptoms of cervical cancer.
“Moving to HPV Primary Screening, and the higher-than-expected HPV and cytology test volumes, has put a lot of pressure on the molecular and cytology teams to process them quickly as possible and provide patients and clinicians with timely and critical information,” says Jenny.
“The lab had to be reorganised to accommodate the new analysers and our staff trained on how they operated for this type of testing, and additional staffing had to be recruited. Intense training was also undertaken by our cytology screeners on interpreting and applying the new clinical management guidelines and reporting guidelines for both swab and cytology results.”
Jenny says the hard work which has gone into launching and running the new programme is delivering results for patients and the lab.
“This screening is accessible and non-invasive and remarkably, in the first six months of the programme, 20 percent of the tests performed across the country were from women who had never been screened, or were outside the screening interval, for cervical cancer.
“The volume of HPV and cytology testing has far exceeded what was expected. Whilst we have faced challenges implementing and running the new programme, we are proud to continue to play a vital role in cervical cancer screening in New Zealand. We expect to see high volumes continuing, and with each swab, another person can screen for early signs of cancer which can provide a great health outcome and save lives,” says Jenny.
