In May 2016 New Zealand, alongside 194 other countries, signed up to the WHO target to eliminate viral hepatitis C as a public health threat by 2030. Despite being very treatable, hepatitis C is often called a silent epidemic due to a lack of obvious symptoms.
While World Hepatitis Day on 28 July is a timely reminder to get tested, more needs to be done to meet this goal. We need to look at how we deliver care differently, and COVID-19 has provided some opportunities to do this.
But the real issue lies in getting tested, or rather that those with hepatitis C aren’t getting tested and therefore aren’t receiving treatment.
About 30-40% of New Zealanders with chronic hepatitis C are undiagnosed because the symptoms aren’t noticeable until 20-40 years later.
If left untreated, up to 25% of infected individuals will develop cirrhosis, or scarring, of the liver, and without successful treatment, 2-5% of those with cirrhosis will end up with life threatening liver cancer or liver failure each year.
So, what is hepatitis C? Hepatitis C is caused by a virus, it spreads through blood-to-blood contact and causes inflammation to the liver.
Those most at-risk of contracting hepatitis C include people who’ve received a tattoo or body piercing using unsterile equipment, had a blood transfusion before 1992, injected drugs or if you’ve received medical treatment in a high-risk country.
While hepatitis C is very treatable – the biggest barrier to receiving treatment is getting diagnosed, as those most likely to be at-risk are also more likely to not get tested.
To combat this Awanui, partnering with Canterbury Health Labs and Te Whatu Ora Health NZ, is trialing a solution.
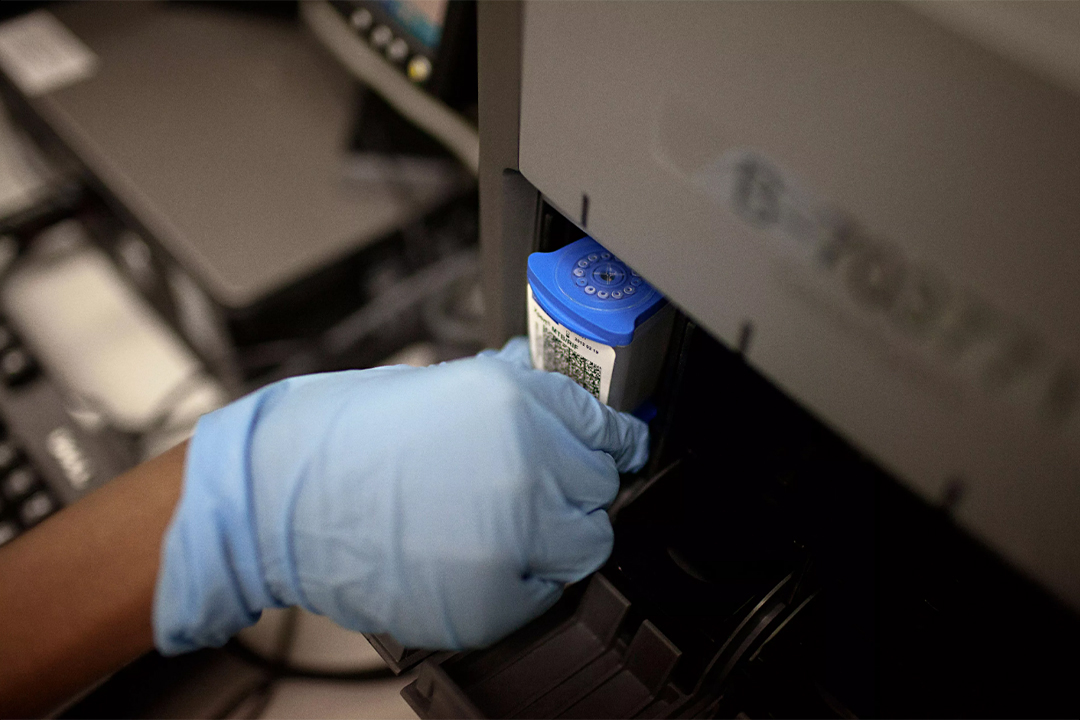
Through a combination of point of care molecular testing technology and information systems, Awanui is working with Canterbury Health Labs and the Southern Region Hepatitis C service to provide a test and treat mobile clinic service. The equipment will be mobile and placed at sites that are frequently visited by our high-risk population, who don’t normally access conventional health services.
The programme is being piloted in Canterbury, with the hope that if its successful it will be expanded to the rest of the country.
Ultimately the aim is to identify hepatitis C patients in high-risk populations and diagnose, assess, and treat these patients in a single visit. This avoids the risk of those who need treatment not returning to receive it.
Our high-risk population include patients who, through lifestyle, environmental or ethnicity have an increased risk of infection and do not access health services in “”normal”” settings. They require a more engaged treatment process.
By moving testing to where patients prefer to access it, a new level of access to hepatitis C treatment can be provided, supporting patients who are currently missed by the traditional health system. We’ll work closely with primary care and community providers and use their networks to target patients.
And to ensure those who need treatment, get it, we’re changing the experience to be a one-stop-shop – not only will patients be diagnosed, but they’ll also receive their treatment at the same place.
COVID-19 and the scale up required to test for it has meant the technology needed to roll out this programme has been deployed around the country. Our laboratories in regions across New Zealand are equipped to analyse tests and turn them around far quicker than before the pandemic.
Viral hepatitis is one of the leading causes of death globally even though it is treatable. Simplifying the process from testing to treatment will help us achieve our goal – a world where everyone living with viral hepatitis has access to safe, affordable and effective treatment.