Genome sequencing had a critical role during the COVID-19 response. It enabled scientists and health experts to track the spread of the virus and when a particular strain was prevalent. A team of Awanui scientists are using the same technology to identify specific strains of bacteria in hospitals in Wellington, Hutt Valley, and Wairarapa.
“Reducing the spread of bacteria between patients is a major challenge for hospitals and health facilities in New Zealand and around the world, particularly when these bacteria are resistant to antibiotics,” says Clinical Microbiologist Max Bloomfield, who is leading the project team.
“Standard methods of surveillance are not very good at picking up outbreaks of these bacteria in hospitals at an early stage. This means outbreaks may get quite large before they are noticed, and it becomes much harder to control them, plus a lot more people may have been affected.”
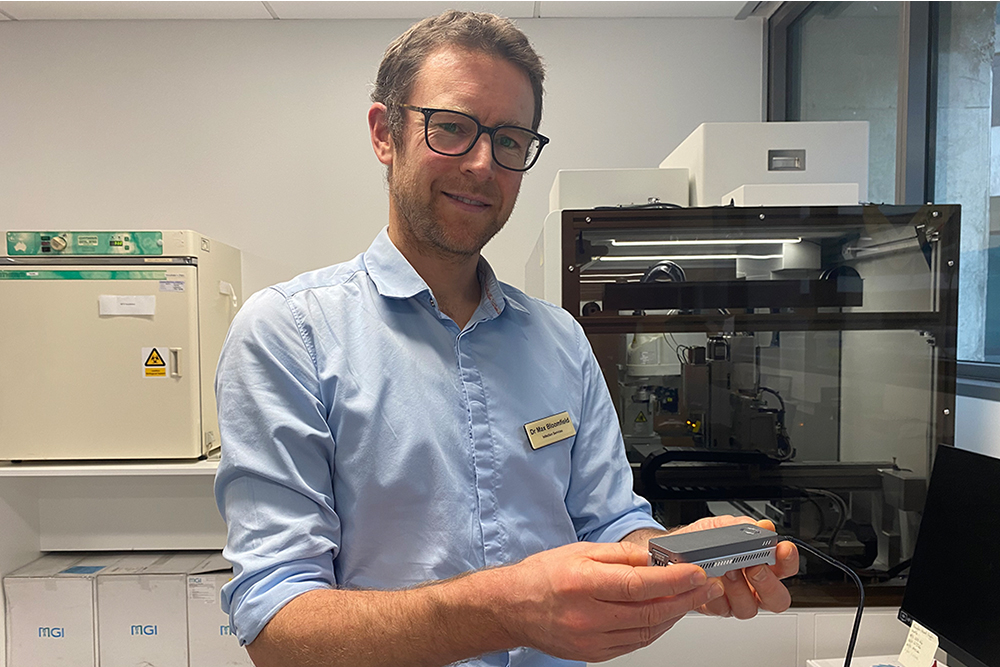
Awanui is using incredible technology called the MinION, which was developed by Oxford Nanopore Technologies. The MinION sequencer fits into the palm of someone’s hand, and plugs into any computer, including a laptop, so in theory can be used anywhere.
“Once bacterial DNA is put into the MinION and analysed, our scientists can know the genetic make-up of the bacteria and see how closely related different strains of bacteria are to each other,” says Max.
“We now routinely perform genetic sequencing on common bacteria known to spread in hospitals, and if we find strains of bacteria which are genetically very closely related in two different patients, it means the bacteria may have been transmitted between them.
“These transmission events can lead to outbreaks, so if we can spot them early when only a small number of patients are involved, we can take action to prevent further spread. This is the same principle used during the COVID-19 pandemic, where ESR was sequencing the virus.”
Since Awanui started this work last year, a significant outbreak of Clostridioides difficile was identified, which can cause diarrhoea in the hospital and can make people very sick. Without genome sequencing it would very likely have gone undetected.
“In one case, we detected a certain sequence type of C. difficile, pinpointing one particular area of the hospital, and the people who had been in this area. After looking at our data, the hospital infection control team made some changes to cleaning practices, and the outbreak was effectively controlled very quickly,” says Max.
The feedback and response from hospital infection control teams for the work Max and the team are doing has been really positive, especially as it has reduced the number of large manual investigations which they have had to do themselves.
“This technology not only allows us to spot outbreaks, but also allows us to be far more accurate when we are trying to respond to the threats some of these bacteria pose to healthcare. It means we can also rule out outbreaks at an early stage too. This can be very important, because investigating an outbreak can be very disruptive to hospital services, so the sequencing can help maintain business as usual.”
Max is also supporting the Awanui team in Dunedin to get this sequencing up and running in the south.
“There is the potential for our team to use genome sequencing around the country and continue working with our hospital colleagues in other centres to respond to a potential infection risk in a targeted and correct way and keep staff, patients and visitors safe.”